Back Next Home Settling down to a new dream June’s diary The bus
isn't crowded like a regular city bus. A few passengers get down at a nearby
stop. A new passenger gets up and eyes me with a hint of recognition. One of my
patient's relatives I presume. The next
bed in the special ward is a 90-year-young Second World War veteran. It has
been years since he left the army and came down to his village, enjoying the
gentle comforts of rural life. His abdomen was distended with fluid in the sac
covering his intestines. This sac was made of a thin layer of cells and had
been also covering his lungs since he was a fetus. At his age of 90 as the
fluid in the sac covering his intestines increased water also seeped into his
lung coverings. The cause of all this water accumulation was off course in his
liver that over the years of dealing with a generous supply of Alcohol had
fibrosed…or did it just age like all other cells of his body? No...Aging
wouldn't cause fibrosis. Whatever it was, all this fibrosis was compressing the
pipes supplying blood to his liver. The rivers inside those pipes were trying
to find other avenues of drainage by trying to percolate into his visceral
coverings. We thought it was alcoholic cirrhosis. We questioned him on his
alcohol habits. He said he did take alcohol and with a wink added it was just
to taste her daughter's home made local brew to make sure the taste was all
right for their guests. As the bus
drove into the lakeside we made our way through a variety of stores selling
items of tourist interest, trekking shoes, sleeping bags, instigating us to
take off into the wild, away from this busy market place. The lake
was calm with a few boats gently drifting in its midst. There was an island
which too seemed to be drifting. A few rain clouds had descended on the
adjoining mountains full of lush green forests, a pagoda stared at us from its
top. We watched our surroundings from a comfortable vantage point near the
lake, inside an open air restaurant, a few buffaloes having a dip, children
diving in to join them with a splash. June felt
relaxed swimming with her colleagues after having taken the plunge into her new
job. She was a consultant trouble shooter now and a teacher-lecturer at that.
Their hospital didn’t lack in system problems. Solving these were at the same
time less taxing as the number of patients wasn’t very high like in city
hospitals. She put all her heart and soul into dealing with them as best as she
could and reveled in the questions asked by her students, an important way to
keep learning. The story of
glomerular injury 1
It has been long since June met Professor
Joatmon in his limestone cave of holistic medicine full of stalactites and
stalagmites. At present if you move these curtains you can spot June looking
smart in that suit, standing on the pulpit with a laser pointer in her hand.
She’s become an Asstt professor herself now, teaching in the June starts off with, “May we have the first slide please?”
The first
slide is a picture of Macchapucchare teaching hospital,
This is
his village where the only means of travel was an airstrip apart from the other
option of a few days of walking
Prem was
intelligent and soon after he finished his 10th grade exams he decided to leave his village for
higher studies. The story of
glomerular injury 2
He came to
Pokhara, enrolled in a good school and saw proper roads and vehicles for the
first time.
As he was
a good student he got into engineering and after finishing his degree, arrived
in US as a software analyst. However he felt miserable there as he kept missing
his relations and his mother’s cooking (among other things). He was actually
relieved when he got the pink slip and lost his job after the economic
slowdown.
He came back to his village (and his mothers
cooking) but found that by now he couldn’t adjust with his brothers who knew
more than him about farming and all his knowledge of software was of no use in
the village (which didn’t even have a single computer) 97 The story of glomerular injury 3
While all
this was happening to Prem our protagonist in his macrocosm, quite unknown to
him or anybody else a major war had already started inside his kidney where his
glomeruli were being attacked by a lot of inflammatory cells.
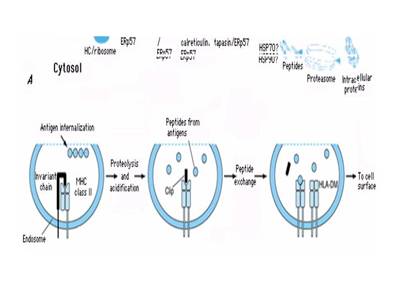
This is a cartoon borrowed from The story of glomerular injury 4
This is
the strong inflammatory response inside Prem Bahadur’s glomerulus as a result
of which we expect to see a lot of protein and RBCs in his urine (if only we
could have examined it earlier). However Prem Bahadur didn’t notice anything
wrong with his urine. His neighbors noticed him growing plump day by day and
complimented him on this sign of prosperity. At first Prem Bahadur was also
happy that he was getting fat but later noticed that he was unable to enjoy his
mother’s cooking due to a feeling of extreme nausea. This too was ignored by
him until one day he developed extreme breathlessness and had to be rushed to
our hospital in Pokhara.
This is a picture of our hospital on a stormy
night. When I saw him in our casualty (for the first time) I found him gasping
for breath, his lungs were full of crepitations which we quickly treated with
Lasix and referred him to
The biopsy
showed focal areas of glomeruli that were sclerosed in segments. The story of glomerular injury 5The fire
was too severe to be quenched with steroids and it was already too late to
prevent Prem Bahadur’s kidney from blowing up in smoke.
He
received a few more dialysis from
The story of
glomerular injury 6
The last I
heard of him was through one of our medical students also from the same
village. Prem was spending his last days in deathbed with his family praying
for him daily and it would be a matter of days or months before death would
take him.
This is a
summary of the story of glomerular injury which describes how it’s initiated by
breakdown of tolerance leading to reactivity of antibodies with planted
glomerular antigens which in turn generates a chemical cytokine mediated
response leading to proliferation of inflammatory cells and subsequent irreversible
renal damage (in a substantial number of people). The story of
glomerular injury 7
The key
word here is tolerance and (next slide)
Tolerance is fast becoming popular in
transplantation research but we need tolerance urgently before the need for
transplantation arises to save our native kidneys (before the inflammatory
cells attack them). As much as we need tolerance to save this Earth before a
full-fledged war breaks out. That is the problem of glomerular injury for we
don’t really know why this breakdown of tolerance occurs. We don’t even know
why hypertension or diabetes occurs (for that matter). Our present strategy is
only to control them in the hope of slowing the progression of renal disease.
Going up and down tops and
bottoms June had
begun the most crucial learning phase of her life that God was looking for.
There were two traditional approaches to learning, the top down and the bottoms
up. Like her friend Paul from the complexity list elaborated in an email, “Top down is a pre-formed idea and we can choose to say yes or no.
Bottom up is an exploratory idea where new direction can be woven from multiple
diverse strands (many of which can be "top down"). Top down is essential;
bottom up is existential. Top down relates to realist ontology - it is really
objectively there; bottom up relates to relativist ontology - it is there if it
is meaningful to you. Today's bottom up can be tomorrow's top down and vice
versa. Top down in one place is bottom up in another. The two are
constantly (and rightly) interwoven at all levels. June's
undergrad years had been more top down assimilating her tools, a knowledge base
accumulated over decades of bottoms up research by physicians of yore. Now was
the time to use the tools she had acquired to fix human systems independently
in a judicious mixture of the two approaches”. Jung
Bahadur Gurung was a retired Indian army soldier who came into her outpatient
chamber with a complaint of fever for a month. For a number of years he had had
severe pain abdomen coming on intermittently for a number of years. He had
yellow eyes that looked quite unwell and he kept scratching his body. June did
a quick system river check and his blood tests indicated an inflamed liver
evidenced by the enzymes. It also suggested the inflammation was obstructing
the outflow of bile from his liver and this was producing all the scratching.
June's gut feeling told her it was a granulomatous inflammation of the liver
possibly due to tuberculosis. Jung
Bahadur was admitted for a liver biopsy after June asked her radiologist friend
to look for and rule out any dilated bile pipes inside the liver that might
suggest a block to the pipes carrying bile into the liver. He took a quick look
with an ultrasound beam and reassured her that the liver pipes were all right.
June went ahead with the liver biopsy and got her liver tissue but was shocked
to find that she was hitting pus. That night the pressures inside Jung
Bahadur’s system rivers hit an all time low at 60 mm of mercury even as his
temperatures swung up to a high of 40 degrees cent and June thought she would
lose him. The commonest complication of a liver biopsy is bleeding from the
liver bed but June was puzzled as his hemoglobin was not dropping. A repeat
ultrasound examination revealed a large sub diaphragmatic abscess that had been
overlooked in the previous ultrasound. June realized she was partly responsible
for this as she had hurried the radiologist into simply ruling out a specific
top down problem and not having allowed him a complete
bottoms up look. Jung Bahadur was operated for the abscess below the
diaphragm and the surgeons also discovered a perforated gall bladder. The pus
had obviously come from an infected gall bladder and the organism was found to
be Salmonella paratyphi. Salmonella getting into the blood stream was a common
cause of fever in this part of the world but this one had got into the gall
bladder, perforated it and caused an abscess manifesting as prolonged fever.
Jung Bahadur followed up with June for years to come after his complete
recovery. Fever bugs in system-rivers Apart from the unusual presentations of
fever the usual fevers were no less interesting. Typhoid was endemic in the
area, possibly as compensation to malaria that was less common. Typhoid meant,
‘like Typhus’, which was less common but present nevertheless. Systems
afflicted had this splitting headache, apathy and loss of appetite. Most
systems malfunctions could be classified into that affecting the system from
outside (bugs getting in through online attachments) or from inside due to the
systems anti-bug defense software gone awry. June got to see more of system
problems due to outside bugs. Fever was indicative of the anti-bug software
working overtime, producing chemicals like lymphokines that when dumped into
system rivers would naturally heat up the system. The commonest bug to cause
seasonal fevers was off course the common cold virus where systems would start
blowing their nose along with sneezing and dripping secretions everywhere. Most
of these malfunctions would be temporary and would subside on their own hardly
requiring any anti-bug software. The Typhoid bug on the other hand would also
produce high grade fever that would characteristically refuse to touch normal
baseline in the first few days. June found monitoring system temperatures by
plotting a 4 hourly graph quite useful in differentiating between viral and
typhoid fevers at least in the initial two or three days. It was all the more
necessary to prevent misuse of anti-bug software in the community. In fact
anti-bug misuse was assuming epidemic proportions in the community far greater
than the bug epidemic. Once anti-bug software was used frequently the bugs
would get to recognize their weak spots and modify their codes accordingly so
they could escape their next onslaught. Most community practitioners, health
assistants and physicians alike resorted to prescribing antibiotics under the
mistaken assumption that they would bring prompt relief. June found it was
paracetamol that would be able to give them better relief. Anti-bugs more often
would just add to the misery by producing diarrhea. She began to design a
prospective trial in the community to see if distributing fever charts to
patients could really help to bring down this present epidemic of anti-bug
misuse. Apart from the common typhoid, June noticed another particularly
different pattern of fevers, as high grade as typhoid. It was however
intermittent in pattern even in the very first days of its appearance and was
remarkably resistant to anti-typhoid software. It would come in epidemics every
monsoon and most people affected were farmers. They had biochemical
abnormalities in the form of raised enzymes in their liver function tests and mild
degree of proteinuria and WBC casts suggesting a
liver and renal involvement. This was Typhus which responded remarkably to
another software, doxycycline. The name Typhoid was
actually derived from Typhus meaning typhoid like and yet Typhoid ruled the roost
as an endemic disease while Typhus was just an epidemic visitor. There were
systems met infrequently that would present with continuous fever where no
amount of investigations would reveal any clue. Very often they would
demonstrate multi-component involvement, be it in the joints, or skin, or
kidney filters, or heart, lung coverings or even the bone marrow affecting
their cell producing assembly lines. Here it was the systems own anti-bug
defense gone awry attacking and corrupting own files. Most of them responded to
software termed immunosuppressive. Sometimes they would respond to
nothing. The cranky irritable bowel June’s diary (draft of a mail to Jo- on her experiences with the irritable bowel)5 My first acquaintance with the disease was possibly at a time when I didn't have any connection with medicine. It began with my father. He was a very meticulous man and was by profession an anthropologist-teacher. His abdomen at that point of time while I was in school oblivious of my future medical career was gradually putting on a paunch. It was not however his paunch that bothered him, it was gas. Gas always used to have ticklish connotations for us young ones probably as it came out from banal orifices producing an offensive sound and odor. However it was not the coming out of gas that seemed to bother him. It was the not coming out part that was most worrisome. He used to feel miserable about his intermittent abdominal bloating, producing a diffuse pain. Very often he would express his anguish by percussing various parts of his abdomen, even while moving around with his daily activities until it became a habit. He even developed a philosophy of happiness which stated that all cause of human misery lay in the abdomen. If only abdominal organs functioned well, everything would be perfectly alright in this world. Surprisingly he grew out of it although it took him years and I no longer find him percussing his own abdomen. I went on to meet similar people in my human trouble shooting career. At first I used to attribute them to protozoan infestations like Giardia or Entamoeba so very endemic in our part of the world but gradually realized that most often no cause could be detected. There were so many criteria to identify the irritable bowel and most of these problem patients would satisfy quite a few. The treatment was however dismal as the cause wasn’t clear. It was a disturbance of bowel movement alright but then why should the bowel move so mischievously at times? A typical scenario was the bowel moving in alternate contraction and relaxations and suddenly at one point of time stopping randomly followed by distension of that halted segment until the human carrying the bowel winced in pain. Mercifully it would pass off after some time, the distended colonic gas coming out silently or otherwise and you’d find a relieved expression on his face. Another way it would present was an urge to defecate at times especially when the subject was engaged in some kind of work, tedious and boring but important nevertheless. However what would come out could hardly be called fecal matter rather than that which was normally present on the surface of the colonic mucus membrane, ‘mucus.’ Each time one passed stools one felt there was more to pass, a sensation termed tenesmus that was possibly due to colonic spasm. Eighty of hundred patients in my outpatient clinic with abdominal pain going on for a very long time could be classified into this pattern. A dysfunctional dyspeptic stomach Vatta- an Ayurvedic
concept: People with predominance of disorders of movement or motion in the
body It was not just the lower bowel whose movement was at fault but even the upper bowel along with the stomach would refuse to budge at times. This produced an upper abdominal epigastric discomfort frequently labeled dyspepsia. June would put in flexible telescopes with lighted lens into these mischievous bowels either from above or below to look for anything that could be treated but no it was something to do with the electrical wiring of their slow moving pipes that wouldn’t move because of frequent current failures. There was no way she could have their wiring replaced. What could have led to their movements getting awry? She decided to drop a mail to her old professor Joatmon. Dear June, Sitting in a busy OPD (with both patients and students) and evaluating dyspepsia (which happens to be one of the commonest patient complaints in the OPD closely rivaling headaches and chest pain) one needs to develop a quick but full proof strategy to evaluate these patients. We had been taught a lot of clinical features to distinguish between duodenal and gastric ulcers in our undergraduate days but what we possibly needed more was to distinguish between ulcer and non- ulcer dyspepsia. Dyspepsia subgroups Reflux-like dyspepsia
Ulcer-like dyspepsia
Dysmotility-like dyspepsia
Setting gas purely unconditionally free There are a lot of clinical subgroups initially devised in the hope of achieving therapy tailored to specific symptoms but they don’t help in distinguishing clinically between ulcer and non ulcer dyspepsia. In fact the only thing, which might give us a clue to an ulcer or an endoscopically verifiable structural lesion, is the presence of recent onset dyspepsia. Patients having symptoms of long-term dyspepsia do generally turn out to have no ulcer disease on Endoscopy. In a Western series, only four out of 165 dyspeptic patients who did not have a peptic ulcer at initial Endoscopy developed an ulcer over 10 years of follow up, although 62 (58%) of the 106 who still had dyspepsia 10 years later had ulcer- like symptoms. What then is the cause of this dyspepsia, which is so very distressing to our patients? If most of them are supposed to have ulcers only when the dyspepsia is recent could it be that the ulcers heal and leave no trace of organic lesion but do cause some neural damage on the long run affecting gastric/bowel function. In many patients, failure of the peristaltic wave to propagate results in upper abdominal discomfort, early satiety or post-prandial fullness (doomma houni) or a sense of gano-gola formation. There are no medicines yet in the market to really improve bowel motility ( Cisapride, metoclopramide and domperidone aren’t practically that effective) , however there may be some benefit in walking after meals, at least this has been demonstrated to improve gastric motility in diabetics. It’s rather surprising that it hasn’t yet been tried or verified in non ulcer dyspepsia. There are many questions, which remain unanswered even in ulcer dyspepsia. Like why does H. Pylori eradication only improve ulcer healing and doesn’t have much benefit in non-ulcer dyspeptics who harbor H. Pylori? Is it because H. Pylori is not really the causative agent of ulcers but only responsible for delayed ulcer healing? I would suggest that you counsel your patients to optimize their bowel movements such that their bowel doesn’t get confused. All they need to do is move it everyday at particular fixed times. In other words eat and pass stools at the same time every day. As these bowels are autonomic and do not directly take orders from the brain they can only be regulated by timely stimuli or signals to their electrical apparatus. Walking regularly in addition would also offer a timely stimulus to their regular movement. Same could be inferred about sleep I guess but all these definitely need to be validated by controlled trials and why don’t you take up the challenge? Jo. A blackening lady One day, June noticed in her outpatient department a middle aged lady who appeared strikingly black, a complexion never noticed in her part of the world. She quickly asked her in and admitted her after a brief history. She was a 40 year old lady from Mustang valley, On physical examination she was cachectic (weighing 30 kgs)
and pale along with diffuse hyper-pigmentation of skin and dorsum of the
tongue. The blood pressure was 84/60 mmHg in the right upper limb and pulse
rate was normal. The abdomen revealed a mild diffuse tenderness and the knee
and hip joints showed bilaterally symmetrical contractures. There were no other
remarkable findings on systemic examination. Her Hemoglobin was 11g/dl and
total leukocyte count was 6,200 with a normal differential count. The serum
sodium was the lower limit of normal at134 mmol/L and the serum potassium was
3.3mmol/L. The liver function tests showed a mild rise of enzymes. The chest
X-ray showed a small calcified focus in the left upper lobe of lung. An
ultrasound revealed a right suprarenal hypo echoic mass posterior to the
Inferior vena-cava, measuring 2.5 X 1.8 X 1.6 cm. Displaced retroperitoneal fat
planes seen between the mass and adjacent liver parenchyma suggested it was an
adrenal mass. There was no similar obvious mass in the left adrenal area. An
ultrasound guided fine needle aspiration was performed which showed frank pus.
This on further microscopic examination showed gram negative bacilli that on
culture grew mucoid colonies indicating Klebsiella pneumonia sensitive to
ciprofloxacin, Gentamicin, Cephazolin,
ceftazidime and resistant to Ampicillin.
The patient was already put on Anti- tubercular therapy after a clinical
diagnosis of A web based doctor patient relationship The patient gave June and her colleagues a lot of surprises. Although C.T scans are known to reveal enlarged adrenals at advanced stages of tubercular Addison's disease, it is not very common to visualize them on ultrasound, let alone do an ultrasound guided fine needle aspiration. To her further wonder it turned out to be pus, which revealed the bug Klebsiella pneumonia as a possible source, hitherto unheard of as producing Addison's disease. There were two possibilities, either it was secondary bacterial infection on top of primary involvement of the adrenals with tuberculosis or it was a primary infection of the Klebsiella Pneumonia involving the adrenal gland. Odd for the bug Klebsiella was the remarkable lack of fever, or any other symptoms to suggest the portal of entry (unless it was the febrile pneumonia like illness she had had 15 years back). However a source could also have been from the urinary tract as Klebsiella is known to cause asymptomatic bacteruria. June posted her experience on a medical web site and one fine day was surprised to receive a mail from another patient long after she had put the whole thing at the back of her mind. Dear
June, I read your case report "A blackening Lady". I found it
interesting. I am
currently treating Klebsiella pneumonia bacterial infection. Would
you please respond with your thoughts on the following question... I'd
struggled with recurring symptoms related to klebsiella infection for the past
15 years. In the beginning of those years, I was suffering with recurring
flu-like symptoms. Bronchial infections began then as well and continued
to return (with the "current jelly sputum"). Urinary tract
infections recurred often, a back problem began 7 years ago and progressively
grew worse...I was told it was termed ankylosing spondylitis. Here's
my question...How long can an overgrowth of klebsiella pneumonia bacteria be
present? Is it reasonable to assume that this has been the underlying
problem for these past 15 years? According to the research I'm finding it
would seem logical, yet I cannot locate any information regarding how long this
overgrowth can remain in the body. The
one mention of that issue was stated "death occurs within 48 hours", I believe that is inaccurate information. Can you
assist me with this question? I'd
greatly appreciate you're response. Chris Jestus,
A web based relationship 2 Thanks for your mail. Could I ask how you
chanced upon my article? Before I attempt to answer your questions I need to
clarify your symptoms in the history. Where was the klebsiella in your
case isolated from? Was it the sputum or the urine? How many times has it been
detected in your sputum/urine? Klebsiella can present in a variety of ways and
our "blackening lady" was one of them. It can present as severe
sepsis where the bacteria continue to divide relentlessly and can definitely
kill a patient in days. However in your case its presentation seems to be what
I understand from your history as a recurrent respiratory tract infection in
which case it’s unlikely that it will do much damage. Please let me know the
details, particularly if there is any finding in your Chest X-ray. Thanks
for writing and do reply for I want to help you solve your problem, yours sincerely Juneli Sen. MD, Asstt Prof, Dept of
Internal Medicine, Phone: 00977-61-26416-extn-189, Fax-00977-61-27862 Dear Juneli, Thank you for
responding. I chanced upon your article by researching
Klebsiella Pneumonia bacteria; I've been looking into many sights to confirm my
belief that the Klebsiella has been the underlying issue in my situation.
I believe, based on the research I'm finding, that it
is possible. The Klebsiella bacterium was detected
through Comprehensive Stool Analysis, through Great Shakes Diagnostic
Lab. Regarding the sputum and urine... the
sputum was never tested, yet in the past have had sputum that was very
concentrated (almost a rubbery consistency, with a
darker color)...recognizably different from the normal phlegm
consistency. I've noticed this when the bronchial infections are
most severe. In past urine tests, E. coli showed
up a couple of times. I'm seeing pictures that show a resemblance to
klebsiella. A webpage that shows the similarities is http://www.mfi.ku.dk/ppaulev/chapter33/images/33-4.jpg
I question if it's possible that klebsiella may have been present. Urinary
tract infections had been recurring at least a few times a month
throughout the years since then. I kept a good supply of cranberry
capsules on hand, as they were often needed. I also consumed a lot of
garlic throughout the years to fight off frequent illnesses. My ongoing struggle with recurring symptoms
began 25 years back. At that time my medical report noted "
diarrhea, cramps, acute viral gastrointestinitis, Leg aches, fibromyalgia
symptoms, blood tests showed neutrophils low (46.7) lymphocytes high (44.2), IgG antibodies". From then on ....I never
felt completely healthy. A
web based relationship 3 I had been prescribed many antibiotics from
that time through 1994...at which time I started researching natural approaches
to help control the many recurring yeast infections, thrush, allergies etc.
(which I understand leads back to overuse of antibiotics). The following notes are taken from my
medical reports.... Over the past 15 years I was to doctors
many times with complaints of overwhelming fatigue, depression, and bronchial
infections that would last for weeks, subside, and then return within a few
weeks again. My blood pressure would usually be on
the low side (98/36, 96/40, 84/60, 80/50 ), I frequently felt ill with
flu-like symptoms, often had low temps as well (97*, 96.4*, 95.7*, 94*); I was having fibromyalgia symptoms
(often aching in various parts of my body, which came and went, recurring in
different areas with each onset, more noticed in the morning). I had chronic constipation
that began in 1993... For the past 10 years I could not pass fecal matter
without an enema and when I did, I often suffered from hemorrhoids and bleeding
from straining. I became too thin and was often told by my husband and friends
that I needed to gain weight. I often felt weak and periodically got
dizzy. Over the past couple of years, I was
becoming more forgetful and struggled with confusion and unclear
thinking. I struggled with manic-depression as well for the past few years.
I also struggled with Pre menstrual syndrome, a lot prior to my monthly cycle
along with recurring headaches often. I would get sore lumps under my armpit
(assuming swollen lymph node). My breast had become continuously
tender and painful for the past year or so. I'd began seeing chiropractors
in 1996 with lower back pain which progressively grew worse, and eventually affected
my entire back and neck, was particularly painful on left side between shoulder
blade and spine. I wasn't able to sleep well, my eyes were often red and I
was told I had Ankylosing Spondylitis. There's a good study
mentioned by the X-ray (1996) L5 sacralized as per
chiropractor. In 2002 another chiropractors notes read "Chris has bone
spurs @ the 4, 5, 6th lumbar vertebra, the 5th lumbar is fused with the
sacrum". Range of motion has fluctuated throughout the years from
30% to 90%...stiffness came and went but continued to grow worse in general. Bone scan (3-16-01) showed right increase
activity in upper left costal vertebra junction at T3 level, noted
possible degenerative activity, no significant abnormalities within the verterbal bodies along with mild scoliosis of thoracic
spine. A web based relationship 4 Chris’s
medical history contd A CT scan ( Echocardiogram ( In regards to helping me solve my
problem...thank you for your interest...I sincerely appreciate that. The above issues have all
significantly improved. (I would say at least 80%). I
now am sleeping well at night; the back pain is very minimal compared to
before. The last bout of severe chest pain was over 3 months ago; I feel
all the psychological issues have been gone since January, I am able to stay
focused and my memory is better; I no longer get urinary tract infections like
I used to, no headaches or P.M.S. symptoms in the past few months; I'm not
aching in various places any more...I wake in the morning without pain.
My eyes are not red all the time; I have no swollen lumps under my arm, my
breasts are not hurting all the time etc. etc. In general...I've come a
long way and I am so very thankful for that. The improvements began to happen when
I began passing long strands of mucous in my stools in November of
2002. I believed they were worms, but two different lab tests
reported no worms. They were defined as "mucoid
matter". (One test was done at a local lab, the other at Great Shakes
Diagnostic Lab…the tests were done about 2 months after I began passing a lot
of these strands) These mucous strands have ranged up to 26"
long. I've preserved some in jars in hopes that someone working in the
research of Klebsiella bacteria would be interested in studying this. I'm
reading that Klebsiella is a highly mucoid bacteria and my doctor had told me
that it is possible that the klebsiella are responsible for these mucous
strands...any thoughts on that? I still continue to pass some of these
mucous strands, much less than at first, but still some. I feel that the Klebsiella is the
underlying issue, but I'd like your opinion...does that seem logical? I
think it does, but I'm not a doctor or specialist. I am so thankful to be regaining my health
in significant ways...I hope that by sharing my experience, it may help others
in some way. Yours Chris Jestus All humans are born physicians June was perplexed initially as to
how she should respond to Chris’s letter as her letter could be obviously
labeled as that of a hypochondriac by contemporary medical school teaching but
then she had also studied in a different school part time. Joatmon’s teachings
in post modern holistic medicine always emphasized that all humans were born
physicians by virtue of their ownership right on their systems. The role of a
formally trained trouble shooter was simply to act as a facilitator in a global
understanding of the nature of the human system and its afflictions. She wrote
back… Thanks Chris, for giving me the opportunity to go through your case
sheet. I believe I have been able to solve your problem. I enclose a paragraph
from Klebsiella species are
broadly prevalent in the environment and colonize mucosal surfaces of mammals.
In healthy humans, K. pneumonia
colonization rates range from 5 to 35% in the colon and from 1 to 5% in the
oropharynx; the skin is usually colonized only transiently. In long-term-care
facilities and hospitals, colonization occurs with K. oxytoxa as well, and carriage rates are significant among
both workers and patients. Person-to-person spread is thought to be the
predominant mode of acquisition. Most of us carry a world of bacteria inside our systems where they
live and die continuing their cycles of existence. Your klebsiella was one such
isolated from your stool where it was living a normal life with minimum damage
to your system. However the troubles which started in your system since 1988
definitely signifies the entry of a virus (something which may be likened to
software programs which affect our computer systems) and it really troubled you
all these days starting from an acute diarrhea, cramps, moving on to Leg aches
and fibromyalgia symptoms followed by constipation which made you suffer
so much. There is nothing in your medical investigations to suggest Ankylosing
spondylitis as the X-ray changes described in ankylosing spondylitis are very
much different from the ones described in your imaging findings. They are non
specific changes possibly normal for your age...by the way I don't know your
age accurately. Although klebsiella antigens are related to ank-spond they are
hypothesized to cause so by acting as a trigger for an autoimmune reaction to
the antigen by the body's cellular defense system. MUCUS is a normal
constituent which layers the bowels of all normal human beings and is passed
out when stools are scanty inside the bowels. The klebsiella is unlikely to
remain alive for this long inside the jars where you have stored them. Yours
June Next Home
Unpublished novel for all interested in the science and fantasy of medicine. Not about religion, but a postmodern multi genre combining elements of Science, Fantasy and Romance |